Tongue Reduction Surgery for Sleep Apnea
How is tongue reduction surgery performed to treat OSA?
 Reducing the tongue with surgery
Reducing the tongue with surgeryDo you have a large tongue? People with tongue size larger than normal can experience breathing difficulties during sleep.
Sometimes, in severe cases, the breathing can stop, causing obstructive sleep apnea.
Tongue reduction surgery can help you eliminate those apnea episodes.
The surgery represents a multitude of methods that can reduce the size of your tongue to a size where you can breathe normally during sleep.
What is Tongue Base Reduction?
This procedure has the purpose to reduce the overall size of the base of the tongue.
As you probably know, the collapsibility of the tongue during sleep is one of the most common causes of obstructive sleep apnea. Having an enlarged base of the tongue is a burden for many of patients with sleep apnea, because every time they sleep on the back, they start snoring or stop breathing during sleep.
In this case, positional therapy is very effective to improve the quality of sleep. However, what if the base of the tongue is so large that sleeping on the side, tongue devices or CPAP can't help you anymore?
This is the situation where the surgery comes to help you...
Tongue Base Reduction Procedure
Who are Candidates for Tongue Reduction?
This procedure is recommended for:
- patients with severe obstructive sleep apnea,
- for those who can't tolerate CPAP,
- or for persons who have a large base of tongue, including patients with macroglossia, or down syndrome.
Diagnosing the Size of Your Tongue
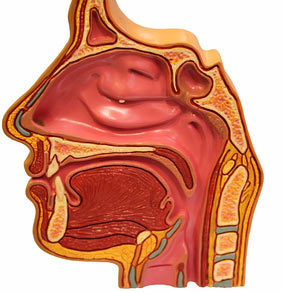
For many doctors it's no mystery that the evaluation for the lower pharynx is the most difficult evaluation. The doctor has to use fiberoptic laryngoscopy or nasolaryngoscopy to investigate the base of the tongue.
The base of tongue is difficult to observe just by opening the mouth. Why? Because you can't see the back part of the tongue that it curves down into the throat.
A trans-nasal fiber optic exam seem mandatory to assess the size of the base of the tongue and its contribution to pharyngeal obstruction during sleep.
How is Tongue Reduction Performed?
The tongue reduction is a direct action on the tongue to treat obstructive apnea. The other surgical methods, such as: geioglossal advancement, hyoid advancement or mandibular advancement, act indirectly on the tongue by moving it forward.
The oral appliance, like the tongue retaining device has also a similar action.
Why is it necessary to move the tongue forward? The reason is to make more space in the pharyngeal zone and to prevent the collapsibility of the tongue in sleep.
There are two main types of tongue reduction surgeries:
1. Resection of the tongue base - tissue cutting
This surgery is performed under general anesthesia, and before treating the tongue base, a tracheotomy or a nasotracheal intubation has to be performed, to ensure breathing.
The surgeon will use a CO2 laser to reduce the tissue from the back of the tongue, avoiding in the same time the tongue musculature.
The bleeding will be coagulated with electrocautery.
2. Base of Tongue Coblation - Radiofrequency Tissue Volume Reduction of the Tongue
Radiofrequency energy has been used for many applications including tissue cutting, vessel coagulation, and tissue volume reduction.
The energy is applied to the tongue base with a needle electrode (Evac T&A Plasma Wand), which is inserted into the tissue.
This radiofrequency energy causes the tissues to heat up, liquified and suctioned out.
The procedure is less invasive than previous method, but it still needs general anesthesia.
After the surgery, you will be asked to sleep with the head elevated, to use intermittent ice application to the tongue for several days, and to use CPAP when sleeping.
You will need several sessions of tongue base coblation (every 4-6 weeks) until snoring and sleep apnea symptoms are eliminated or improved).
This video shows you how the radio frequency base tongue reduction is performed:
Success Rates for Tongue Reduction
Several studies have shown a range between 20 to 80% success rate, where patients with a larger amount of tissue resected have a higher improvement rate.
Combined with other surgeries for sleep apnea, like UPPP or mandibular advancement, the rates of success can increase.
Here are some examples of such studies:
- Tongue Base Suspension Combined with UPPP in Severe OSA Patients,
- preliminary clinical results of tongue-base suspension with a soft tissue-to-bone anchor for obstructive sleep apnea.
Complications of Tongue Reduction Surgery
Tongue paralysis
Tongue paralysis may be possible only if the surgery affects the nerves of the tongue (hypoglossal nerves).
That's why the surgeon will mark the area with a skin marker to prevent touching these nerves. However, you may feel after the surgery temporary weakness of the tongue, but this is very rare.
Loss of sense of taste
You can lose the sense of taste if the mucosa of the tongue is injured, or the lingual nerves are affected.
Dysphagia
Dysphagia is only temporary due to limitation of the tongue motion and scar formation.
Tissue edema
Ttissue edema is a risk for airway obstruction. This is the reason for taking steroids during tongue reduction recovery (as well as practicing head elevation and using the CPAP): to reduce the edema quickly and to maintain the airway open.
Home › Sleep Apnea Surgery › Tongue Reduction







